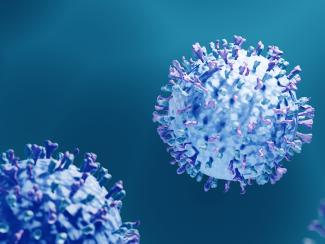
Researchers studied the virus using 3D peripheral nerve cultures grown from stem cells and rat embryos. After finding they can be infected by RSV, researchers found RSV induced the release of chemokines — proteins that fight infections by controlling immune cells — and caused significant inflammation.
With low levels of RSV infection, the nerves became hyperreactive to stimulation. At higher levels, they observed a progressive degeneration of the nerve and increased neurotoxicity due to excess inflammation.
“Until this study, the theory was that the inflammatory response was indirectly activating the nerves,” Piedimonte said. “This study shows that not only does that happen, but the virus can penetrate directly into the nerves.”
The nerve hyperreactivity could explain why children who get RSV are more likely to have asthmatic symptoms later, Piedimonte said.
The study also found that RSV could enter the spinal cord via peripheral nerves despite not having the ability to enter the spinal neurons directly. More research is needed to explore that mechanism, but Piedimonte theorizes that by using the peripheral nerves to enter the spinal cord, RSV can bypass the blood-brain barrier, enter the central nervous system and infect the brain.
If confirmed, it could signal a connection between RSV and other neurological or developmental disorders, Piedimonte said.
“If indeed it’s confirmed in future studies that viruses like this are able to access the central nervous system, that opens a huge Pandora’s box,” Piedimonte said.
Co-authors on the study include Michael Moore, PhD, Kevin Pollard, PhD, and Alexander Bosak of Tulane’s School of Science and Engineering’s Neural Microengineering Laboratory; Vicki Traina-Dorge, PhD, of the Tulane National Primate Research Center; Dr. Gregory Bix, director of the Clinical Neuroscience Research Center; and Stephen Medearis of Tulane School of Medicine.